Introduction
The management of glenoid deformity continues to evolve as has the sophistication of its evaluation. With the assistance of preoperative planning precise evaluation of multiplanar glenoid deformity is possible. Imprecise recognition and/or inaccurate correction of complex glenoid deformities can lead to malpositioning of the glenoid implant increasing the risk of failure. Failures can be due to aseptic loosening as a result of increased glenoid component shear forces, decreased range of motion and scapular notching. In addition, without glenoid deformity correction theoretical biomechanical benefits of lateralization and soft tissue tensioning are not realized. Current management strategies including eccentric “high-side” reaming as well as structural bone grafting can compromise existing anatomy and carry high failure rates.
Summary
The purpose of this study was to evaluate the difference in functional outcomes, range of motion, complications, and revision rates between augmented and standard baseplates in RSA for patients with significant posterior or superior glenoid wear. The authors of this multicenter study were able to demonstrate improvement in multiple clinical outcomes without a difference in complication or revision rates with the use of baseplate wedge augmentation compared to standard baseplates. This study adds to the growing body of literature in support of baseplate augmentation.
Materials and Methods
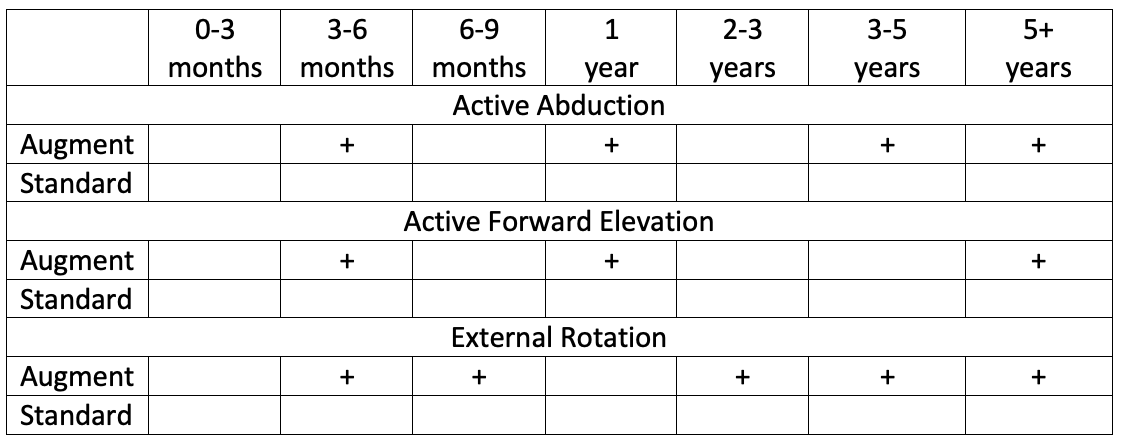
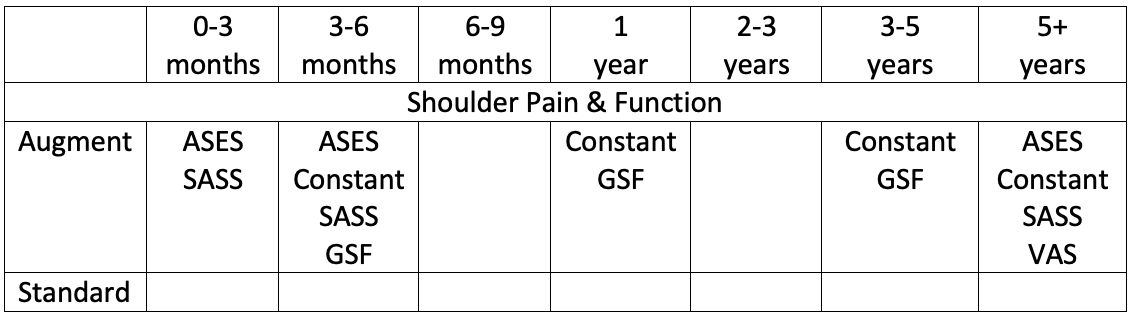
A multicenter retrospective analysis of 171 patients with glenoid bone loss who underwent RSA with and without augmented baseplates was performed using the Equinoxe single platform shoulder prosthesis. The multi-center clinical outcomes database was analyzed which resulted in 171 RSA patients with a diagnosis of rotator cuff deficiency with identified significant posterior or superior wear. Of the 171 RSA patients 84 received standard baseplates and 87 received augmented baseplates (14 superior, 47 posterior, and 26 posterior/superior augments). Of the 171 RSA performed only 9 were performed using preoperative planning software and GPS navigation. All 9 GPS patients were within the augment cases. Range of motion (active abduction, active forward elevation, active external rotation, and active internal rotation), shoulder pain and function (VAS pain score, global shoulder function score, Constant score, ASES score, and the Shoulder Arthroplasty Smart outcomes scores) were quantified preoperatively and at each postoperative visit (0-3 months, 3-6 months, 6-9 months, 1 year, 2-3 years, 3-5 years and 5+ years). Postoperative complications and revisions were recorded.
Results
The augment cohort were greater in age (73.3 vs 70.0 years) and preoperative glenoid retroversion (17.4 vs 9.1 degrees). The standard cohort had greater preoperative forward elevation (98 vs 80 degrees), and internal rotation scores (3.3 vs 1.9), whereas preoperative abduction and external rotation did not differ. There were no differences in preoperative shoulder pain and function scores between cohorts.
Augment group demonstrated significantly greater improvements (+) in postoperative ROM, and shoulder pain and function scores compared to the standard group at several follow up time points.
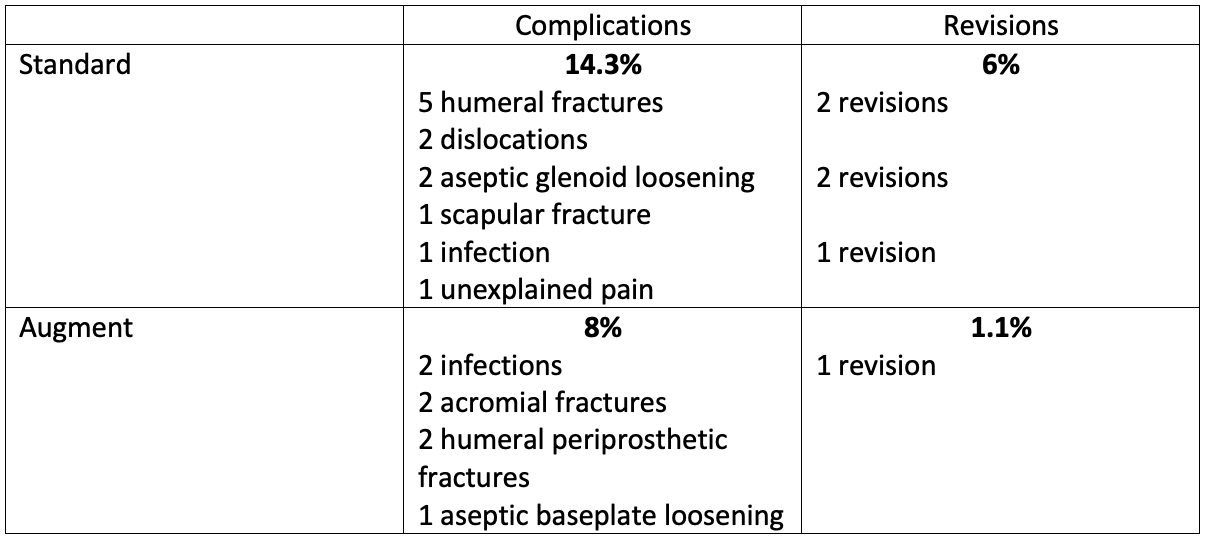
Overall complications (19) and revisions (6) were low. The most common complication was periprosthetic fracture, whereas the most common indications for revision were glenoid baseplate loosening, infection and humerus fracture. There was a trend nearing significance for higher revisions within the standard baseplate cohort.
Discussion
Augmented baseplates allow the surgeon to correct glenoid sided deformity while maintaining glenoid bone stock, optimizing the biomechanical advantage of lateralization and remaining soft tissues while avoiding graft related complications. This comparative study demonstrated that the augmented cohort achieved significantly higher postoperative shoulder function scores and greater ROM improvements from baseline. The results of this study, despite significantly greater preoperative glenoid retroversion than the standard cohort, validate the use of augmented baseplates in the setting of RSA and glenoid deformity.
Reviewer Comments
This study is the largest study to date using augmented baseplates in deformed glenoids, strengthened by the use of a multi-center database. This adds to the growing body of literature supporting the use of the Equinoxe single platform shoulder prosthesis. Equinoxe Augmented baseplates minimized the risk of glenoid component malposition resulting in fewer complications and revisions, while improving ROM and PROMs as compared to standard baseplates for RSA for patients with rotator cuff deficiency and significant posterior or superior glenoid wear.
