Patients who have undergone total shoulder arthroplasty prefer greater surgeon involvement in shared decision making
Introduction
Traditionally the patient-physician relationship consisted of two most used models: the paternalistic and the informative models. The paternalistic model limits patient autonomy as the physician makes decisions for the patient. Whereas in the informative model decision making is solely up to the patient and the physician’s role is to educate the patient. Over time the patient-physician relationship has evolved into a blend of these two models, the shared decision-making model (SDM). SDM has become the predominate mode of patient-physician interaction allowing for mutual exchange of information throughout the decision-making process. The physician educates the patient on risks, benefits, and alternatives. The patient educates the physician on their values and preferences. SDM allows the two parties to come to a mutually agreed-on decision [1].
Summary
The purpose of this study was to evaluate overall patient preference for SDM and determine demographic and socioeconomic factors related to SDM preference in those undergoing total shoulder arthroplasty. The authors of this retrospective cross-sectional survey demonstrated that patients had a significant preference for surgeon-led decision-making regarding day of surgery decisions, contrary to those decisions associated with the day of surgery and postoperative care. This study adds to the understanding of the concept of SDM.
Materials and Methods
A retrospective, cross-sectional study enrolled patients who had undergone a primary anatomic or reverse total shoulder arthroplasty between the ages of 40-89 years. All patients completed a 2-part questionnaire.
Data collected in the 1st portion included:
- Age
- Sex
- Race & Ethnicity
- Highest level of education
- Household pretax annual income
- Type of health insurance
- Preoperative diagnosis
- Type of primary shoulder arthroplasty
- Treating surgeon
Questions in the 2nd portion pertained to the decision-making process and scored on a –5 to 5 scale as follows:
| -5.0 to –1.7 | Increased surgeon involvement |
| -1.7 to 1.7 | Shared decision making |
| 1.7 to 5.0 | Patient decision making |
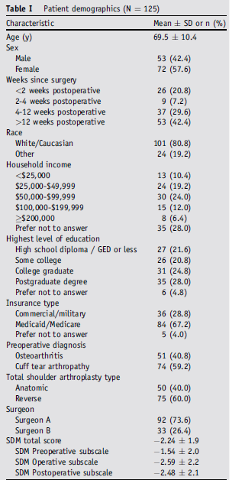
Analysis indicated no significant association between either total or subscale SDM score for the following: age, sex, race, income, education level, insurance, preoperative diagnosis, arthroplasty type, or provider. Significant differences were observed only with preoperative SDM subscale score with a similar but non-significant trend in total SDM and the operative and postoperative SDM subscales.
Discussion
The benefits of patient satisfaction, improved QOL measures, higher satisfaction, and less regret in patients when shared decision making model is employed has been reported in the hip, knee, and spine literature [2]. Based on the questionnaires administered in this study, interestingly, patient preference for a shared decision-making model pertained to preoperative factors such as diagnostic modalities, timing, and treatment options. Whereas the findings indicated a significant preference for surgeon-led decision-making regarding day of surgery decisions (i.e., type of arthroplasty, antibiotic prophylaxis, type of sutures) and postoperative care.
Reviewer Comments
For the most part patients have more resources and access to information about their health. As this study demonstrated there was no significant correlations between SDM scores and age, sex, race, income, education level, or insurance type. Anecdotally, the findings of this study parallel my practice experience. Preference sensitive decisions exist more so preoperatively. I find that during preoperative visits most patients are engaged in mutual exchange. This engagement has led to improved surgical decision making and ensured the trust for me, as the surgeon, to lead decision making intra and postoperatively.
References:
- Wilson, C. D., & Probe, R. A. (2020). Shared decision-making in orthopaedic surgery. JAAOS-Journal of the American Academy of Orthopaedic Surgeons, 28(23), e1032-e1041.
- Sepucha, K. R., Atlas, S. J., Chang, Y., Freiberg, A., Malchau, H., Mangla, M., … & Cha, T. (2018). Informed, patient-centered decisions associated with better health outcomes in orthopedics: prospective cohort study. Medical Decision Making, 38(8), 1018-1026.
