Referenced article: Patients who have undergone total shoulder arthroplasty prefer greater surgeon involvement in shared decision making
A critical juncture of the physician – patient relationship occurs during the intimate discussion regarding surgery. In the past, discussions often revolved around the surgeon making unilateral decisions regarding patient care considering evidence regarding postoperative clinical and radiographic outcomes. More recently however, medicine has transitioned towards more patient centered models taking into consideration patient preferences and values with insurance reimbursement possibly correlated with these patient reported outcomes. Therefore, the importance of patient satisfaction and shared decision making between the physician and patient now has greater implications for surgeons.
Medicine has transitioned towards more patient centered models taking into consideration patient preferences and values with insurance reimbursement possibly correlated with these patient reported outcomes.
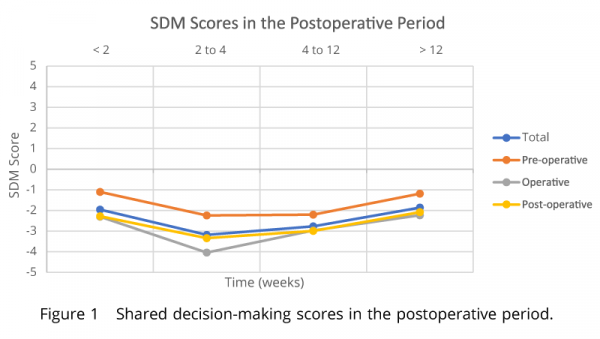
This retrospective cross sectional observational study of primary total shoulder arthroplasty patients evaluated the overall patient preference for shared decision-making. Post-operatively, patients received a 2-part validated questionnaire centered on sociodemographic factors and how they felt about the pre-, op-, and post- operative shared decisions making process. A Scale from -5 to 5 was utilized with 0 being complete shared decision making (fig 1). All scores fell within the -5 to 0 range indicating the authors found that the patients always preferred a greater surgeon led approach but there was a trend towards more shared decision making for the pre-operative period (Fig 2).
This article re-enforces the importance of the pre-surgical discussion with patients. While patients want to feel included in the decision making, I believe the desire for surgeon’s taking the lead for decisions in this population is due to the lack of knowledge in the general population regarding shoulder arthroplasty and the difference between primary and reverse shoulder arthroplasties. While hip and knee replacements have been around decades longer than shoulder arthroplasties, the general population awareness of shoulder replacement surgeries are limited. During my interactions many patients are not aware of shoulder arthroplasties, let alone the difference between a primary and reverse shoulder replacement. Additionally, many of these patients present thinking they will be getting a rotator cuff repair. A significant amount of time is spent explaining the etiology of their condition as well as the difference between shoulder replacements and the difference between a replacement and rotator cuff repair. It is natural that patients want to understand why they may be requiring a reverse shoulder replacement, when they were just told they have a rotator cuff tear by their PCP. It is my responsibility to educate them on the other issues including possible severe arthritis and potentially a massive irreparable rotator cuff tear that could contribute to their symptoms. I do find that once patients understand their underlying problems and options, they put the trust in surgeons to make the best decision for their individual conditions. In conclusion, in my practice it is important to spend the appropriate amount of time with pre-surgical patients to explain the etiologies as well as options. Once they are comfortable with an agreed plan of care, they will entrust me to make the right decisions to carry out that plan.
Fig 1
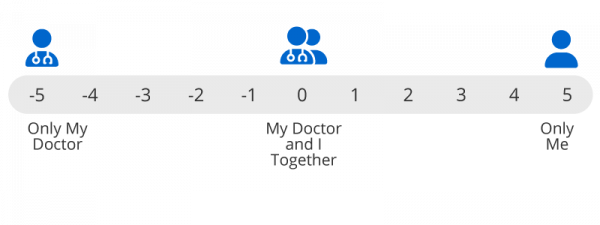
Fig 2