Stress fractures of the acromion and scapular spine remain a vexing complication of reverse shoulder arthroplasty (RSA) as they may substantially impact the final outcome of the procedure particularly when displacement occurs.
A recent publication by the ASES Complications of Reverse Shoulder Arthroplasty Multicenter Research Group reported that these fractures occur in 4-5% of cases overall with a higher risk in female patients, those with osteoporosis and with cuff tear arthropathy or massive rotator cuff tear.(1) Other possible contributory factors that have been suggested include: rheumatoid arthritis, superior baseplate screw placement, violation of the superior shoulder suspensory mechanism, previous shoulder surgery, prosthesis design, and excessive humeral distalization.
These fractures can occur at any time after RSA but most commonly occur in the first several months during which time patients are making the greatest gains in their postoperative recovery. Levy has contributed greatly to the classification of these fractures along with recommended treatment strategies based on their location and displacement.(2) Nevertheless, outcomes after these fractures regardless of treatment are likely never as good as if the fracture never occurred. To this end, a better understanding of the impact of cumulative risk factors in advance of surgery may help surgeons predict those patients at highest risk and consider mitigation strategies to reduce this risk.
Roche et al recently published a multicenter report on the impact of accumulating risk factors on these fractures using a single platform prosthesis with a medialized center of rotation and lateralized humeral prosthesis.(3) The authors confirmed that female gender combined with advancing age and rheumatoid arthritis collectively led to a higher risk of fracture. The authors concluded that it is important to look at different combinations of risk factors to quantify fracture risk rather than looking at each risk factor in isolation.
In this multicenter analysis using standardized data collection and complication reporting of this prosthesis, the overall rate of fracture was 1.52% which included all diagnoses and demographic groups. This series documents one of the lowest reported fracture rates in the literature and this result is strengthened by the large cohort of 9079 patients. A previous study by Routman et all using the same implant documented a fracture rate of 1.77% which is substantially less than the ASES Research Group.(4)
One possible explanation for this lower fracture rate may be the design of the prosthesis which incorporates a medialized glenoid and lateralized humeral configuration. The medialized glenoid respects Grammont’s original design criteria. Unlike Grammont’s design however, the implant used in these studies (Exactech Equinoxe, Exactech, Inc, Gainesville, FL) uses an anatomic head cut with an onlay humeral design which lateralizes the rotation axis of the humerus from the point of articulation of the glenosphere with the humeral insert.
The effect of this combined medial glenoid, lateral humerus (MGLH) is to optimize the deltoid moment arm while improving deltoid wrap around the tuberosity. A longer deltoid moment arm requires less deltoid force to do the work of elevating the arm thereby improving the mechanical advantage of the prosthesis. Allowing stability through deltoid wrap also reduces the deltoid tension that results from excessive distalization as may occur with a Grammont style implant. The graph below, credited to Hamilton et al’s work studying muscle moment arms as a function of reverse implant design, shows that the middle deltoid moment arm of this design is optimized over those that use an inlay humeral implant with a lateralized glenosphere.(5)
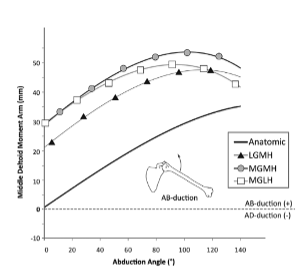
Collectively, these findings suggest that surgeons should consider the cumulative impact of risk factors on fractures of the acromion and scapular spine after RSA. Implant design may be one risk mitigation strategy for high risk patients, and the data from large cohorts suggests that the Equinoxe MGLH design has one of the lowest incidences of fracture based on its biomechanically optimized design.
References:
- ASES Complications of RSA Research Group:, Mahendraraj KA, Abboud J, Armstrong A, Austin L, Brolin T, et al. Predictors of acromial and scapular stress fracture after reverse shoulder arthroplasty: a study by the ASES Complications of RSA Multicenter Research Group. J Shoulder Elbow Surg. 2021 Oct;30(10):2296–305.
- Levy JC, Anderson C, Samson A. Classification of postoperative acromial fractures following reverse shoulder arthroplasty. J Bone Joint Surg Am. 2013 Aug 7;95(15):e104.
- Roche CP, Fan W, Simovitch R, Wright T, Flurin PH, Zuckerman JD, et al. Impact of accumulating risk factors on the acromial and scapular fracture rate after reverse total shoulder arthroplasty with a medialized glenoid-lateralized humerus onlay prosthesis. J Shoulder Elbow Surg. 2023 Jul;32(7):1465–75.
- Routman HD, Simovitch RW, Wright TW, Flurin PH, Zuckerman JD, Roche CP. Acromial and Scapular Fractures After Reverse Total Shoulder Arthroplasty with a Medialized Glenoid and Lateralized Humeral Implant: An Analysis of Outcomes and Risk Factors. J Bone Joint Surg Am. 2020 Oct 7;102(19):1724–33.
- Hamilton MA, Roche CP, Diep P, Flurin PH, Routman HD. Effect of prosthesis design on muscle length and moment arms in reverse total shoulder arthroplasty. Bull Hosp Jt Dis 2013. 2013;71 Suppl 2:S31-35.
