Throughout the field of orthopaedics, there is a trend moving toward preserving as much of the patient’s natural anatomy as possible. Likewise, having access to a wide range of bone conserving implants affords the surgeon the opportunity to treat each patient with respect to anatomical preservation.
In shoulder arthroplasty, understanding the benefits of innovative, canal-sparing humeral implant options brings new considerations in treatment including patient demographic, surgical time and returning patients to post-operative lifestyle in concert with their expectations. Incorporating innovative implants that surgeons believe will improve patient outcomes requires thoughtful consideration and a respect for the required learning curve.
Rick Papandrea, MD, and Stephanie Muh, MD, two fellowship-trained surgeons, share their newly-acquired knowledge—choosing bone-conserving, canal-sparing humeral implants. In the following case reports, they juxtapose patient selection with surgical experiences and outcomes.
“With the advent of shorter stems, I have come to analyze my longer-term follow-up with more scrutiny, and thusly now select shorter stems more frequently, bone quality permitting, due to concerns of proximal stress shielding of the tuberosities. Though I am not sure what length of the shorter style stem is the best choice, I believe the stemless [implants] will be incorporated far more frequently whenever the bone is good enough. I have been able to continue to use an LTO (lesser tuberosity osteotomy) on these cases. Lately, I have only used the standard length stem with significant osteopenia proximally.”
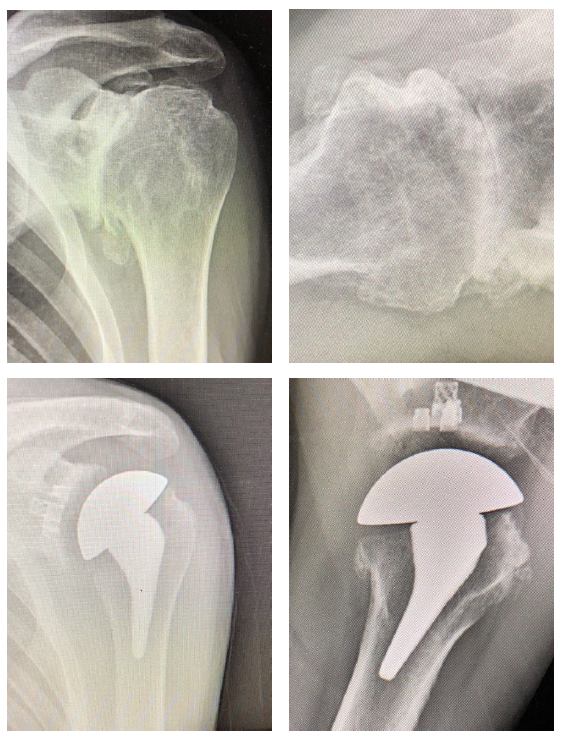 Patient 1: Primary anatomic total shoulder arthroplasty using Equinoxe Preserve short stem and caged glenoid.
Patient 1: Primary anatomic total shoulder arthroplasty using Equinoxe Preserve short stem and caged glenoid.
- Active male in his 60s, retired reporter with surprisingly good preop motion
- This patient is a good candidate for either a stemless anatomic or a short stem anatomic
- Six (6) weeks postop his external rotation (ER) has returned to preop baseline of 45 degrees and his forward flexion (FF) has improved from 90 to 145 degrees.
 Patient 2: Primary anatomic total shoulder arthroplasty using a stemless implant.
Patient 2: Primary anatomic total shoulder arthroplasty using a stemless implant.
- Active male in his 60s, retired radiologist
- Typical pain and significant range of motion limitations
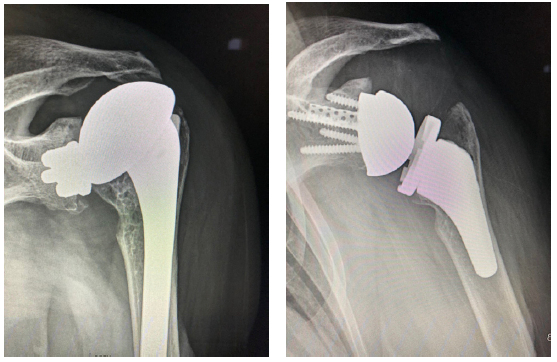 Patient 3: Revision of a failed anatomic total shoulder with loose humeral stem to reverse total shoulder arthroplasty
Patient 3: Revision of a failed anatomic total shoulder with loose humeral stem to reverse total shoulder arthroplasty
- The humeral stem was loose, so it was replaced with the short stem for the aggressive proximal geometry, which fit nicely and improved the proximal press-fit
- Revised an anatomic to a reverse, replacing stem from another company
- Significant glenoid wear led to augmented baseplate choice – superior posterior augment
“I try to use the Equinoxe® Preserve short stem as my primary stem of choice. The only time I will use the standard length stem is if the patient has poor osteoporotic bone during surgery. Generally, I will start with a Preserve preparation, and if I have to broach to a size 8 or larger, I am considering a transition to the primary length stem for better fixation.
Moving from standard to short stem is surgeon-friendly, avoids reaming the canal and is a simple technique. As a surgeon, you have to be cautious and pay close attention to the broach technique so that the stem does not go into varus or valgus.
The short stem has become my primary stem of choice. It is a platform stem allowing for future revisions from TSA to rTSA, avoids reaming the canal, which I believe increases postoperative pain in patients. The short stem allows for more bone preservation for revisions. In my practice, I have also noted there appears to be less proximal osteolysis/resorption as compared to competitor implants. I will also use the stemless implant for very young patients who I am concerned will require multiple revisions in the future.”
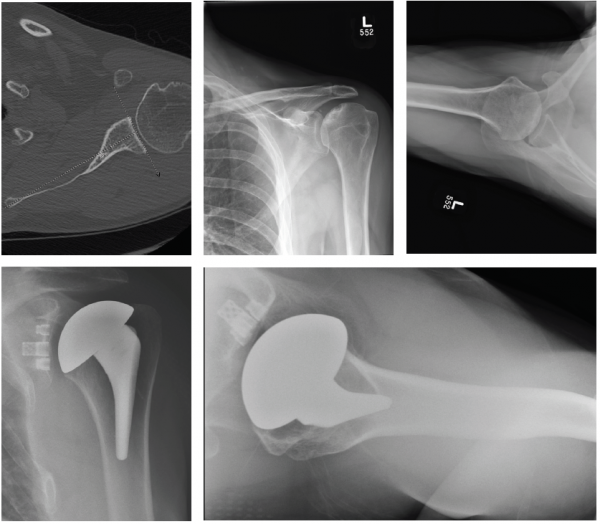 Patient 1: 59-year-old male with avascular necrosis of the humeral head.
Patient 1: 59-year-old male with avascular necrosis of the humeral head.
- Left primary anatomic total shoulder arthroplasty using Equinoxe Preserve short stem and cage glenoid.
 Patient 3: 74-year-old female with cuff tear arthropathy.
Patient 3: 74-year-old female with cuff tear arthropathy.
- Right primary reverse shoulder arthroplasty with augmented baseplate to treat glenoid wear.
![“With the advent of shorter stems, I have come to analyze my longer-term follow-up with more scrutiny, and thusly now select shorter stems more frequently, bone quality permitting, due to concerns of proximal stress shielding of the tuberosities. Though I am not sure what length of the shorter style stem is the best choice, I believe the stemless [implants] will be incorporated far more frequently whenever the bone is good enough. I have been able to continue to use an LTO (lesser tuberosity osteotomy) on these cases. Lately, I have only used the standard length stem with significant osteopenia proximally.” Patient 1: Primary anatomic total shoulder arthroplasty using Equinoxe Preserve short stem and caged glenoid. Active male in his 60s, retired reporter with surprisingly good preop motion This patient is a good candidate for either a stemless anatomic or a short stem anatomic Six (6) weeks postop his external rotation (ER) has returned to preop baseline of 45 degrees and his forward flexion (FF) has improved from 90 to 145 degrees. Patient 2: Primary anatomic total shoulder arthroplasty using a stemless implant. Active male in his 60s, retired radiologist Typical pain and significant range of motion limitations Patient 3: Revision of a failed anatomic total shoulder with loose humeral stem to reverse total shoulder arthroplasty The humeral stem was loose, so it was replaced with the short stem for the aggressive proximal geometry, which fit nicely and improved the proximal press-fit Revised an anatomic to a reverse, replacing stem from another company Significant glenoid wear led to augmented baseplate choice – superior posterior augment Patient 1: 59-year-old male with avascular necrosis of the humeral head. Left primary anatomic total shoulder arthroplasty using Equinoxe Preserve short stem and cage glenoid. Patient 3: 74-year-old female with cuff tear arthropathy. Right primary reverse shoulder arthroplasty with augmented baseplate to treat glenoid wear. Patient 4: 63-year old male with osteoarthritis. Left primary anatomic total shoulder arthroplasty using Equinoxe Preserve short stem with 8-degree cage glenoid.](https://www.exac.com/wp-content/uploads/2023/10/63-year-old-male-with-osteoarthritis.png)
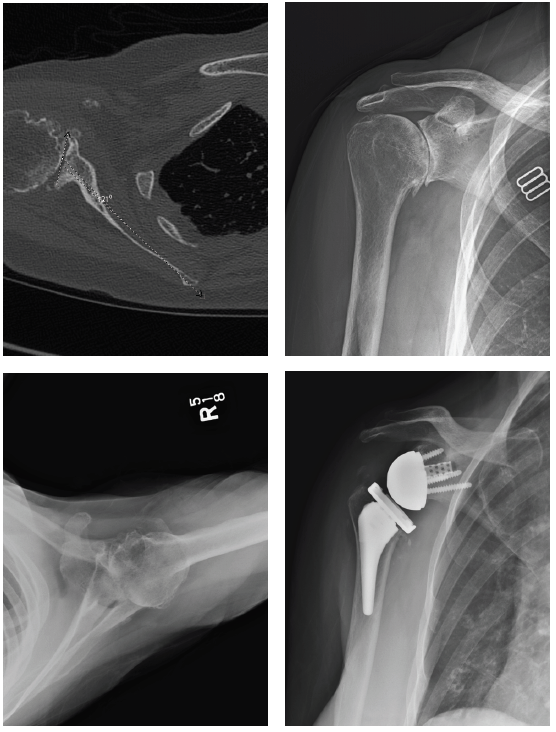
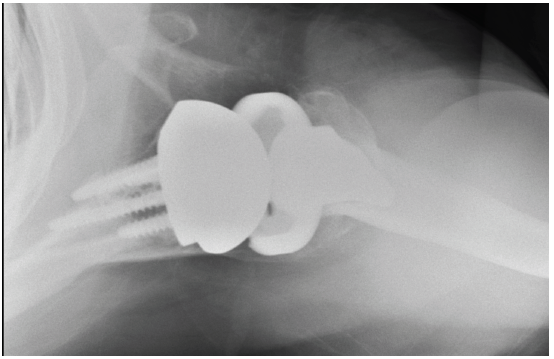
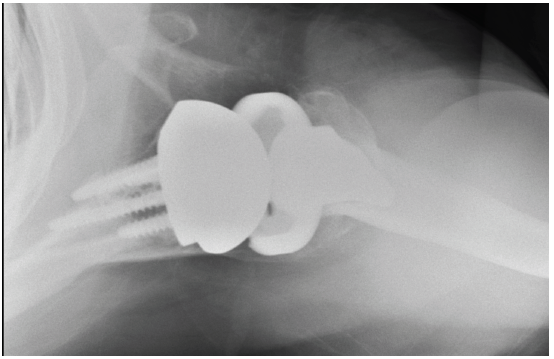 Patient 4: 63-year old male with osteoarthritis.
Patient 4: 63-year old male with osteoarthritis.
- Left primary anatomic total shoulder arthroplasty using Equinoxe Preserve short stem with 8-degree cage glenoid.
