Gregory Gilot, MD
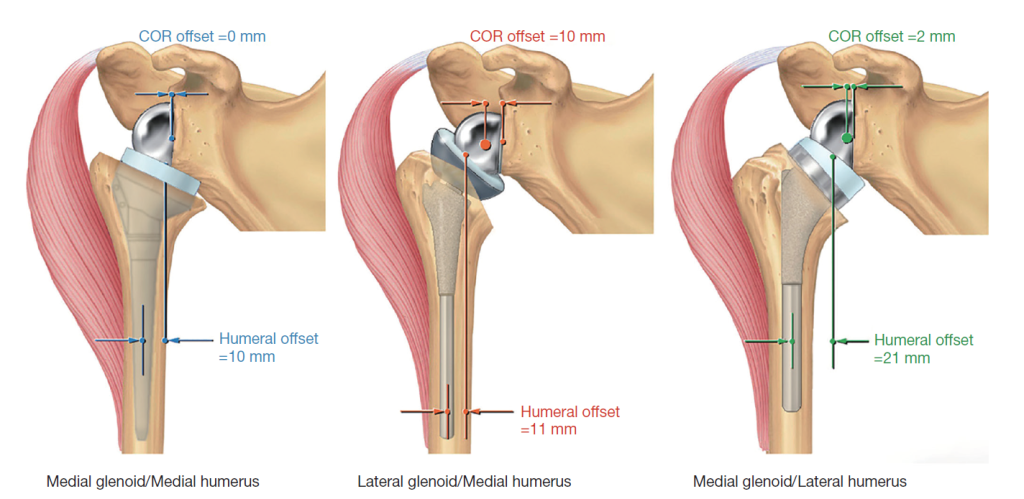
The FDA approved the use of the reverse shoulder prosthesis in the United States in 2004, nearly 25 years following its re-debut in France. Combined, there are 40 years of experience addressing varying shoulder conditions once treated with non-prosthetic or unconstrained shoulder arthroplasty solutions. Surgical techniques and prosthetic designs have evolved over the years, leading to improvements in clinical outcomes, implant longevity and lower rates of complications. The earliest design, the Grammont-style reverse shoulder arthroplasty (RSA), was built on the engineering premise of a medialized center of rotation, as measured at the center of the glenosphere, in reference to the native glenoid face. While a medialized center of rotation increases the mechanical efficiency of the deltoid, it tends to result in mechanical impingement between the humeral polyethylene insert and the scapula neck. Cadaveric and biomechanical studies as well as computer simulation models have demonstrated the increased risk of the following complications: scapular notching, decreased rotation and prosthetic instability; whereas a lateralized center of rotation has demonstrated superiority in maximizing overall passive arc of motion and preventing scapular notching. In addition, the tensioned soft tissues (remaining rotator cuff and deltoid) effectually improve implant stability.1,2
Surgical lateralization can be achieved via metal or bone. Using a thicker baseplate and/or glenosphere achieves glenoid sided lateralization while increasing joint loading. The increased compressive and shearing forces increases the potential for glenoid loosening.3 To offset the torque forces seen in metallic increase offset (MIO-RSA), bone graft can be placed under the baseplate; and once healed, theoretically, the center of rotation is lateralized and remains at the bone-implant interface.
In a study by Boileau et al, a retrospective case series of 143 shoulders were treated with a BIO-RSA for rotator cuff deficiency.4 It was a multicenter retrospective study with a minimum of five years’ follow-up. All patients in the study had a Grammont-style RSA with the use of autograft harvested from the humerus for bony lateralization. The mean follow-up period was 75 months, the preoperative diagnosis varied, the average age was 72 years, and 72% were women. Patients undergoing revisions or those with insufficient humeral head autograft were excluded. From a technical standpoint, a cylinder of cancellous bone was harvested from the humeral head of 7mm and 10mm thickness, for 42mm sphere and 36mm sphere, respectively, and placed on the baseplate. All baseplates were implanted with a lengthened central peg in 10° of inferior tilt.
Post-operative clinical and radiographic assessment was performed. Constant score, ROM, strength, VAS and SSV were measured preoperatively and at each follow-up. Post-op X-rays and CT scans were analyzed for: (1) bone graft healing, (2) bone graft viability, (3) baseplate fixation, (4) inferior scapular notching, (5) inferior glenoid spurs, (6) glenosphere inclination, (7) glenosphere inferior overhang, (8) humeral component fixation, and (9) greater tuberosity resorption.
Overall BIO-RSA was found to be effective. Ten (10) percent experienced complications, of which 4% underwent revisions. Three cases involved glenoid loosening with graft failure. Overall scapular notching rate was 56%, and 18% experienced severe scapular notching. This risk correlated with lower BMI and glenoid malposition. There was a 53° gain in anterior elevation and 13° for external rotation. Constant score and SSV improved to 93 and 77, respectively. Mean VAS was 2. Both implant survivorship and graft incorporation were at 96%. Lastly, 83% were satisfied or very satisfied.
Despite the positive outcomes, this study demonstrated that glenoid lateralization was insufficient in eliminating scapular notching. Three parameters were found to be significantly associated with scapular notching: (1) thin patients with low BMI; (2) <5mm of glenosphere inferior offset; and (3) >5° of superior inclination. The high rate of patient satisfaction, patient reported outcomes, low glenoid failure rates, and dislocation rates seen in this study are equivalent to those observed in patients undergoing lateralized MIO-RSA. This is believed to be accomplished by tensioning the remaining rotator cuff muscles and improving the deltoid wrapping mechanism.
This is another example of a clinical study that draws conclusions about the Grammont-style design limitations and the techniques and modifications required for improved outcomes. Glenoid grafting or technical modifications that result in lateralization of the center of rotation, glenoid overhang and/or correction of inclination are technical and not inherent to implant design. In my practice, I employ such techniques when utilizing more medial implant designs. What is interesting in this study is despite the 7-10mm of bone graft required for lateralization, scapular notching remained high at above 50%. It appears that, as this study highlights, Grammont-style designs inherently lead to some extent of inferior scapular impingement, mechanical abutment of the humeral poly, and inferior scapular neck leading to scapular notching, which in this study was noted to be severe in nearly 20% of patients. I suspect that the humeral design and neck inclination also play a part in humeral abutment. Medial and inferior humeral placement is mechanically inferior.
A number of studies have reported minimal scapular notching achieved with prosthetic designs featuring a lateralized glenosphere (MIO-RSA) or a lateralized humeral design. One of these is the Equinoxe® Shoulder System, which is a lateral humeral/medial glenoid design.5 With only 2mm lateral offset built into the glenosphere, the majority of the lateral offset is obtained with humeral lateralization via an onlay humeral design onto an anatomic humeral neck cut. These design factors uniquely place the humerus in a mechanically favorable position. This provides for a low rate of scapular notching, which has been demonstrated in a study by Simovitch et al,6 showing a 14.5% scapular notching rate in 324 patients assessed at an average of 75 months follow-up.
 In conclusion, BIO-RSA is an effective technique to achieve excellent functional outcomes, high patient satisfaction, and decrease post-operative complications namely, scapular notching. The take-home message is that thin patients are at risk for developing scapular notching; care to correctly place the baseplate in neutral inclination with sufficient glenosphere inferior offset can further minimize scapular notching; and lastly, implant designs that achieve lateralization via the glenosphere or humeral lateralization appear to be superior in reducing the risk of scapular notching.
In conclusion, BIO-RSA is an effective technique to achieve excellent functional outcomes, high patient satisfaction, and decrease post-operative complications namely, scapular notching. The take-home message is that thin patients are at risk for developing scapular notching; care to correctly place the baseplate in neutral inclination with sufficient glenosphere inferior offset can further minimize scapular notching; and lastly, implant designs that achieve lateralization via the glenosphere or humeral lateralization appear to be superior in reducing the risk of scapular notching.
References
- Bassens D, Decock T, Van Tongel A, De Wilde L. Long-term results of the Delta Xtend reverse shoulder prosthesis. J Shoulder Elbow Surg. 2019 Jun;28(6):1091-1097. doi: 10.1016/j.jse.2018.11.043. Epub 2019 Feb 1.
- Roche C, Flurin PH, Wright T, Crosby LA, Mauldin M, Zuckerman JD. An evaluation of the relationships between reverse shoulder design parameters and range of motion, impingement, and stability. J Shoulder Elbow Surg. 2009 Sep-Oct;18(5):734-41. doi: 10.1016/j.jse.2008.12.008. Epub 2009 Feb 27.
- Stroud NJ, DiPaola MJ, Martin BL, Steiler CA, Flurin PH, Wright TW, Zuckerman JD, Roche CP. Initial glenoid fixation using two different reverse shoulder designs with an equivalent center of rotation in a low-density and high-density bone substitute. J Shoulder Elbow Surg. 2013 Nov;22(11):1573-9. doi: 10.1016/j.jse.2013.01.037. Epub 2013 Apr 10.
- Boileau P, Morin-Salvo N, Bessière C, Chelli M, Gauci MO, Lemmex DB. Bony increased-offset-reverse shoulder arthroplasty: 5 to 10 years’ follow-up. J Shoulder Elbow Surg. 2020 Oct;29(10):2111-2122. doi: 10.1016/j.jse.2020.02.008. Epub 2020 Jun 4.
- Hansen ML, Routman H. The biomechanics of current reverse shoulder replacement options. Annals of Joint. 2019;4:17-17. doi:10.21037/aoj.2019.01.06.
- Simovitch R, Flurin PH, Wright TW, Zuckerman JD, Roche C. Impact of scapular notching on reverse total shoulder arthroplasty midterm outcomes: 5-year minimum follow-up. J Shoulder Elbow Surg. 2019 Dec;28(12):2301-2307. doi: 10.1016/j.jse.2019.04.042. Epub 2019 Jul 13.
