Rick Papandrea, MD
Orthopaedic Associates of Wisconsin
Although considered cutting edge only a few years ago, outpatient total shoulder arthroplasty (TSA) has now become routine at some facilities. What follows are some current thoughts, as well as recent past experiences of the author performing total shoulder arthroplasty in an outpatient setting.
In this article, outpatient total shoulder arthroplasty will include both same day discharges and 23-hour overnight stays. Total shoulder arthroplasty, whether an anatomic, or reversed implant, is deemed an inpatient procedure by Medicare. Therefore, total shoulder arthroplasty cannot be done at an outpatient facility for a Medicare patient. This review will not consider any specifics of the Medicare population for that reason.
Over the past four years, this author’s ambulatory surgery center has performed 369 total shoulder arthroplasties. One hundred seventy nine were anatomic devices, 190 were reversed devices. Before embarking on outpatient total shoulder arthroplasty, both the surgeon and facility must consider the necessary components required for both a safe and successful program.
Surgeons who desire to utilize such a program should first have the skill set to reliably and efficiently perform total shoulder arthroplasty. There needs to be confidence in not only completion of the procedure, but the awareness necessary to predict in whom the procedure can most efficiently and effectively be carried out. Surgeons who routinely require prolonged operative times, especially for glenoid exposure might want to consider honing their skills set prior to performing outpatient arthroplasty. Likewise, the surgeon must be cognizant of the challenging factors that make certain patients more appropriate in a hospital setting. Severe bone loss, significant stiffness, and obesity are all reasons to give pause when considering patient selection. The surgeon must be completely aware of, and confident in the capabilities of the specific arthroplasty system chosen.
Over the past four years, this author’s ambulatory surgery center has performed 369 total shoulder arthroplasties. One hundred seventy nine were anatomic devices, 190 were reversed devices.
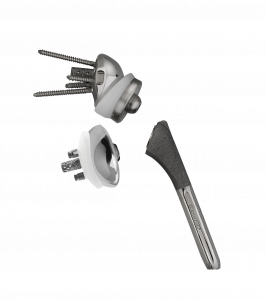
I have found the Exactech Equinoxe® system ideal for outpatient arthroplasty due to the extreme flexibility it provides. When utilizing the anatomic system, a backup with the reverse system will allow treatment of unexpected severe rotator cuff pathology, or glenoid deficiency and deformity. Augmented glenoid components, both reverse and anatomic, have essentially eliminated the need for bone graft. This not only saves time in the operating room, it limits the additional equipment and support needs of the facility.
When planning and implementing a shoulder arthroplasty service at an outpatient facility the support staff, the surgeon, and the implant representative need to be aware of, and in sync with the ancillary equipment needs. There needs to be clear understanding of any potential need, such as alternative retractors, cerclage fixation for iatrogenic fractures, polymethylmethacrylate and associated delivery systems for unexpected fixation needs.
Although it may not be the first thought or consideration, insurance reimbursement must be understood prior to initiation of a program for outpatient shoulder arthroplasty. Many, if not most commercial contracts will include arthroplasty, consisting of CPT codes 23472, 23473, and 23474. The contracted reimbursement may or may not be sufficient to cover the overhead of the procedures. In our experience, some contracts needed to be revisited, with special carve out for these codes, prior to initiating the outpatient arthroplasty program. Having an accurate knowledge of local reimbursement rates at the hospital, by specific payors, allows for efficient and effective negotiation of outpatient reimbursement rates. Prior to initiating discussions with payors, it is helpful to obtain EOBs, or explanation of benefits forms, from patients who have undergone total shoulder arthroplasty at an inpatient facility locally. Collecting as many of these as possible will allow the surgeon and outpatient facility to formulate a competitive negotiation plan.
During the same time that the surgeon and facility are considering their ability to carry out outpatient shoulder arthroplasty, and make it financially viable, they need to be considering their physical needs.
The physical needs of the facility extend beyond the operating room. Of course, the procedure must be able to be safely, efficiently, and effectively performed in the operating room. Considerations beyond the operating room include the potential need for additional imaging, the potential for physical therapy, food service needs and recovery needs.
We have found that image fluoroscopy is sufficient for imaging in the operating room, and that it is only needed if there is concern for fracture during the case. In review of my inpatient procedures, I found that postoperative xrays, obtained in the recovery room, did not change the postoperative course of the patient. I have not been obtaining postoperative images routinely in the outpatient setting, although if one desired to do so, current mini c-arms are sufficient.
Having physical therapy see the patient prior to discharge is something that can be considered, if the facility has therapy on site, or therapy is going to visit the patient. There could be some advantages to this, especially if there is a desire to capture the patient for outpatient therapy at a specific facility postoperatively.
We have found that it is quite effective to have the patient watch a pre-recorded video of exercises prior to discharge, they can review at home prior to their first follow up as well. This home-based program has been well received, is convenient, and at times patients differ on going to formal therapy. Recent studies have shown equivalence in home therapy or formal therapy after shoulder arthroplasty.5
Planning should include consideration for the length of recovery period for a patient to be considered outpatient, Medicare rules dictate that an outpatient must be discharged 23 hours or less after they were admitted. Admission is the time of check into the facility, not the time of discharge from PACU. While these rules are Medicare based, it is our experience that commercial providers follow them.
One possible initial plan for outpatient total shoulder arthroplasty is to discharge all patients home on the same day. This obviates the need for any overnight facilities, limits food service needs, and—if the patients are recovered the same as non-arthroplasty outpatients—additional staffing needs are mitigated. This can be accomplished in a few patients, without regional anesthetic, but for the great majority most likely would require regional anesthesia. Single shot scalene blocks have the issue of wearing off in less than one day. This may cause difficulty with the patient being discharged with no pain, and then struggling with pain control at home, often in the evening hours. Patient satisfaction may suffer, there may be increased opportunities for admission or emergency department visits. Indwelling scalene catheter will eliminate this problem, but opens the possibility of other problems such as injury to the anesthetic limb,
noncompliance due to lack of pain, and the potential for anesthetic complications from the block. While complications from regional anesthetic are rare, local anesthetic nerve toxicity is dose and time dependent.1,3,6,7
We decided to initiate our program with a 23 hour, overnight stay. This requires the facility to have overnight capacity which is not only structural, but staff based. Staffing needs may be accommodated with local staffing agencies, or providing bonuses to pre-existing staff. The evening staff must start when the routine shift is done. We have found having a single nurse with ancillary help is effective for one to two patients. If we have three to four patients we have additional staff. The ancillary help with typical utilize is an EMT. We have maintained 2:1 or 1:1 staff-to-patient ratio overnight. This is obviously much higher than done in the hospital setting. This provides not only safety, but high satisfaction.


Figure 1. Routine postoperative dressing utilized by the author for all total shoulders. 1a:
Immediate appearance in the operating room. Note the blanching due to epinephrine in the local
anesthetic injected at the start of the case. This case had enough oozing that a single drain
was placed exiting posterior, through the deltoid, with a separate Tegaderm. 1b: This is a typical
appearance of a postoperative Tegaderm at the time of removal, two weeks from surgery.
We decided to initiate our program with a 23 hour, overnight stay. This requires the facility to have overnight capacity which is not only
structural, but staff based.
Most outpatient facility centers will not have on-site food services for full meal preparation. We have found that a stocked pantry is well received by patients, when combined with local food delivery from multiple restaurants.
Our shoulder arthroplasty program has given us the opportunity to contemplate much of what we do for all our shoulder arthroplasty patients. Improvements made prior to the onset of outpatient shoulder arthroplasty made it possible to consider sending patients home the day after a shoulder replacement. Additional improvements have made the process even more reliable and effective. Continued improvements have benefited both inpatient and outpatient shoulder arthroplasty, in both Medicare and commercial payor populations.
All shoulder arthroplasty patients now receive multimodal pain management. Pre-operative treatment with transexamic acid (TXA), gabapentin and MS Contin, combined with intraoperative Tylenol and Toradol gives excellent pain control, even without a block. Use of a scalene block, with or without an indwelling catheter, has been left to the discretion of the surgeon and patient. I choose to limit the use of blocks, as I find they are typically not necessary for an effective recovery and will not allow for nerve exam postoperatively. Additionally, they will often limit active use for commencement of exercises. If there are plans to stay overnight regardless, I also feel that the block will not give as much time for the patient, with the guidance of nursing, to accommodate the postoperative pain that does occur. I do also have concerns that the block that has just worn off may delay discharge within the necessary 23-hour window.
My protocol for mitigating infection risks include some maneuvers that have ancillary benefits helpful for same or next day discharge. My post-operative bandage has evolved and is now quite aligned with outpatient shoulder arthroplasty.
Patients are instructed to prescribe with Hibiclens the night before and day of surgery. Additionally, I have recently added a daily prep with benzoyl peroxide for three days to decrease skin colonization with Propracnesionibacterium acnes. At surgery, skin preparation starts with an alcohol wash, followed by Chloraprep. Ioban is used to cover and seal the entire shoulder. The incision is injected with 1% lidocaine with epinephrine, not only for some analgesia, but also for hemostasis. One gram of Kefzol is dissolved in the local, to help sterilize the intradermal layer.2,4 This, combined with the TXA makes for minimal blood loss and typically no need for a drain. The skin is closed with asubcuticular closure with Monocryl, and sealed with Dermabond. Tegaderm is applied directly over the incision. This has multiple benefits. The incision can be monitored. The Tegaderm is left in place for two weeks, and has an excellent seal due to the skin prep and lack of bleeding. Typically, the Tegaderm does not come off until it is removed at the first visit at 14 to 15 days. It is waterproof and patients can shower and even swim. This has high acceptance from the patients. They are pleased there is no need for a bandage. The appearance makes for a less “severe” appearing wound, which I believe adds confidence to the patient leaving a facility less than 23 hours after a shoulder replacement.
The growing experience of outpatient shoulder arthroplasty has confirmed that it is safe and effective. Value in healthcare has been defined as outcomes over cost. There is no doubt that outpatient shoulder arthroplasty has, and will continue to provide value to our patients.
References
1. Hogan, Q. H. Pathophysiology of peripheral nerve injury during regional anesthesia. Reg Anesth Pain Med 33:435-441. 2008.
2. Lee, M. J., P. S. Pottinger, S. Butler-Wu, R. E. Bumgarner, S. M. Russ, and F. A. Matsen, 3rd. Propionibacterium persists in the skin despite standard surgical preparation. The Journal of bone and joint surgery 96:1447-1450. 2014.
3. Lenters, T. R., J. Davies, and F. A. Matsen, 3rd. The types and severity of complications associated with interscalene brachial plexus block anesthesia: local and national evidence. J Shoulder Elbow Surg 16:379-387. 2007.
4. Matsen, F. A., 3rd, S. Butler-Wu, B. C. Carofino, J. L. Jette, A. Bertelsen, and R. Bumgarner. Origin of propionibacterium in surgical wounds and evidence-based approach for culturing propionibacterium
from surgical sites. The Journal of bone and joint surgery 95:e1811-1817. 2013.
5. Mulieri, P. J., J. O. Holcomb, P. Dunning, M. Pliner, R. K. Bogle,
D. Pupello, and M. A. Frankle. Is a formal physical therapy program
necessary after total shoulder arthroplasty for osteoarthritis? J Shoulder Elbow Surg 19:570-579. 2010.
6. Verlinde, M., M. W. Hollmann, M. F. Stevens, H. Hermanns, R.
Werdehausen, and P. Lirk. Local Anesthetic-Induced Neurotoxicity.
Int J Mol Sci 17:339. 2016.
7. Werdehausen, R., S. Fazeli, S. Braun, H. Hermanns, F. Essmann,
M. W. Hollmann, I. Bauer, and M. F. Stevens. Apoptosis induction by different local anaesthetics in a neuroblastoma cell line. Br J Anaesth 103:711-718. 2009.
